This week, Highpoint Health laid off 31 employees (less than 5% of the workforce) and reduced the hours of 50 employees, 23 of whom will move to part-time.

(Lawrenceburg, Ind.) - Highpoint Health, like many rural hospitals across the nation, is facing significant financial challenges. This includes an increase in expenses, a decrease in patient volume, a reduction in reimbursements alongside a higher number of uninsured patients and increased regulatory burdens.
“We’ve already taken decisive action aimed at enhancing our revenue cycle, reducing expenses and exploring growth opportunities,” said Michael Schwebler, President and CEO of Highpoint Health. “However, a significant decrease in patient volume has made it necessary for us to rightsize our workforce. This decision was made only after careful consideration and will not affect the high-quality care we provide our patients.”
This week Highpoint Health laid off 31 employees (less than 5% of the workforce) and reduced the hours of 50 employees, 23 of whom will move to part-time.
“Our hearts and prayers go out to the employees affected by this reduction in force,” said Schwebler.
Departing employees will receive severance pay based on length of employment, tuition assistance to the end of the current semester, and either conversion or portability for voluntary term life. Highpoint Health is also working with St. Elizabeth Healthcare and WorkOne Southeast to help displaced employees find jobs. For employees whose hours have been reduced to part time, Highpoint Health is offering health insurance for three months at the full-time rate.
Schwebler attributes the decrease in patient volume to a changing healthcare delivery system. More and more procedures that were inpatient are performed in an outpatient setting. Additionally, increased competition has significantly impacted the number of patients admitted to Highpoint Health.
“Equally as challenging as rising costs and a decrease in patient volume is the ongoing challenges we face getting reimbursed for the services we provide,” said Schwebler. “While this problem certainly isn’t unique to us, rural hospitals do treat a population that tends to be older, poorer and sicker when compared to national averages.”
According to Schwebler, this means Highpoint Health relies more heavily on reimbursements from Medicare and Medicaid, which pay below the cost of care. Not to mention, rural hospitals have the same regulatory burden as other hospitals, despite lower patient volumes. Ultimately, the price for compliance is often higher than for larger, urban facilities.
“We’re proactively addressing our challenges so Highpoint Health can continue to deliver quality and affordable care to our community,” said Schwebler. “By reducing costs, we can continue to achieve our strategic objectives, remain financially stable and grow well into the future.”
 The Community Project Receives $1,000 Grant from DCF
The Community Project Receives $1,000 Grant from DCF
 BCEF's Student Success Center Opens at Batesville High School
BCEF's Student Success Center Opens at Batesville High School
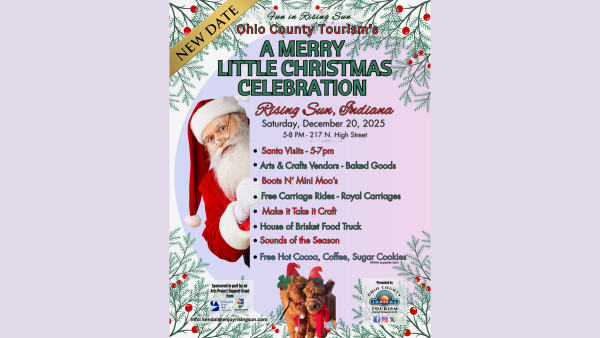 Ohio Co. Tourism Reschedules Merry Little Christmas Celebration
Ohio Co. Tourism Reschedules Merry Little Christmas Celebration
 Indiana Senate Rejects Redistricting Bill
Indiana Senate Rejects Redistricting Bill
 OCCF Names Lilly Scholarship Recipient
OCCF Names Lilly Scholarship Recipient