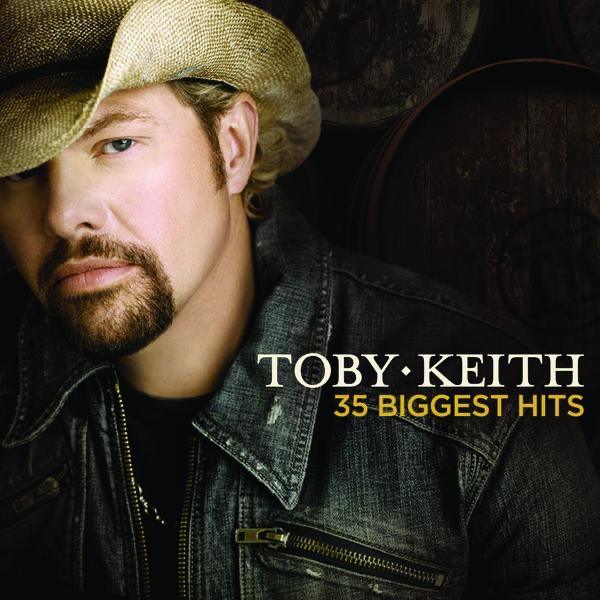
Gov. Holcomb made the announcement Monday afternoon.

(Indianapolis, Ind.) - Governor Eric J. Holcomb announced today that Indiana has received approval to continue its successful alternative to traditional Medicaid expansion—the Healthy Indiana Plan (HIP)—for ten more years. This allows the state to continue health coverage for more than 572,000 low-income adult Hoosiers.
“Today’s extension empowers more than half a million Hoosiers to continue receiving quality health care coverage from our innovative HIP program,” Gov. Holcomb said. “As a national model for a state-led, consumer-driven approach, HIP helps Hoosiers experience improved health outcomes and better lives.”
Additionally, the approval from the U.S. Centers for Medicare and Medicaid Services grants five-year extensions of some of the newer components of Indiana’s HIP program that have provided treatment for substance use disorder and serious mental illness for 88,000 Hoosiers across all Medicaid programs.
“Hoosiers have led on state healthcare innovation for years, including under former Governor Mike Pence and continuing today under Governor Holcomb,” said U.S. Department of Health and Human Services Secretary Alex Azar. “This ten-year extension of the successful Healthy Indiana Program allows the state to make new progress on the kind of patient-centered healthcare system President Trump envisions. State innovation is an opportunity to test out ideas for delivering our ultimate goal of better health and well-being, and we encourage states to continue working with us, like Indiana has, to tailor their programs to their unique needs.”
HIP is a platform for certainty during the pandemic. Members continue coverage during a public health emergency and all cost sharing has been suspended. The program engages members to be active participants in their health care coverage. In 2018, members made more than 545,000 visits for preventive services, and mammograms and vaccinations are at record highs for members. The program combats Indiana’s top contributor to chronic disease – smoking – by waiving copays and covering all therapies.
In a direct effort to support mothers and their babies, HIP Maternity provides full health coverage services – including prenatal services, dental, behavior health, and substance use disorder treatment – at no cost to the member for the duration of her pregnancy and 60 days postpartum. Enrollment in pregnancy management programs increased at an average annual growth rate of 41 percent from 2015 to 2018.
“With this approval, our health policy leaders at FSSA will be able to spend more time operating, evaluating and improving HIP, as well as engaging members and partners,” said Jennifer Sullivan, M.D., M.P.H., Family and Social Services Administration secretary.
HIP was created in 2007 under then Gov. Mitch Daniels. The program was expanded in 2015 by then Gov. Mike Pence with a federal waiver to cover any eligible adult as an alternative to traditional Medicaid expansion.
Typically, the state’s waiver to renew HIP is reviewed and approved every three to four years. Today’s approval runs through December 2030. It marks the first time the federal agency has approved a state’s Medicaid waiver for a comprehensive health benefits program for a period of ten years.
Earlier this year, CMS approved the HIP Workforce Bridge program, which establishes a new, unique transitional phase for HIP members. As they return to the workforce and to employer insurance or other health coverage, members can continue to use their HIP POWER accounts, which are similar to a health savings account.
Learn more about the state’s program and approval at www.HIP.in.gov.
 Bill to Welcome Illinois Counties to Indiana Heads to Governor's Desk
Bill to Welcome Illinois Counties to Indiana Heads to Governor's Desk
 Indiana's Unemployment Rate Drops in March
Indiana's Unemployment Rate Drops in March
 Road Closure Scheduled in Osgood for Crosswalk Installation
Road Closure Scheduled in Osgood for Crosswalk Installation
 Volunteers Needed for Litter Clean-Up on State Line Road
Volunteers Needed for Litter Clean-Up on State Line Road
 Resurfacing Project Scheduled on Airport Access Road
Resurfacing Project Scheduled on Airport Access Road
 Superintendent Writes Letter Regarding Manchester Elementary School Closing
Superintendent Writes Letter Regarding Manchester Elementary School Closing